What is a Claim ID Number?
Every insurance claim in your PCC system has a unique identification number. The number appears in various reports and programs, and you can use it to improve claim tracking and payment posting.
Claim ID Creation and Tracking
As soon as a claim is submitted, PCC's Partner practice management system creates a unique claim ID. The number is submitted on the claim, along with the patient's account number. It should appear on all claims, both electronic or paper, though some insurance carriers occasionally have trouble distinguishing the numbers.
When you are working to track down a problematic claim, you can see the claim ID number in the Correct Mistakes (oops) program, as well as the Account History (tater) report and many other programs. You can also search through your Electronic Claim Submission (ECS) reports (ecsreports) for a specific claim number.
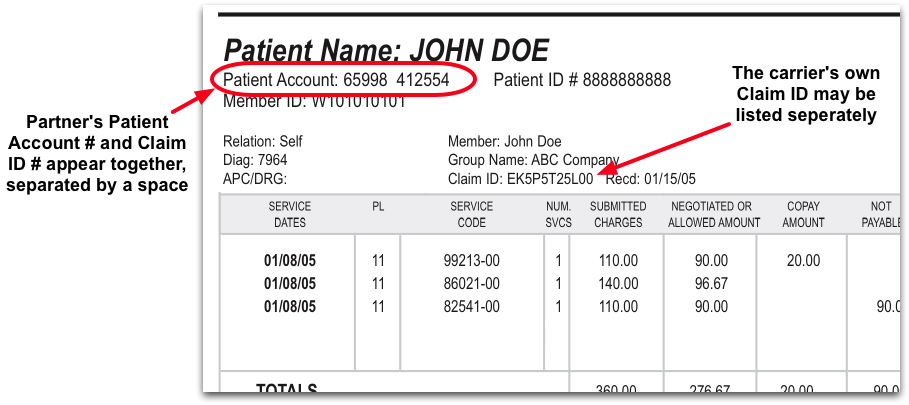
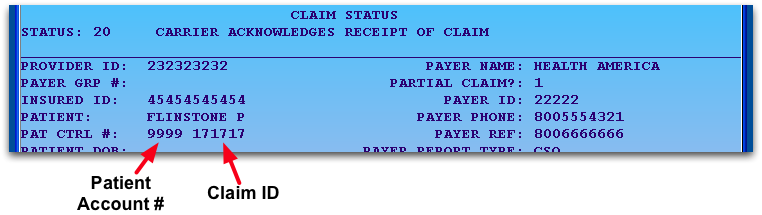
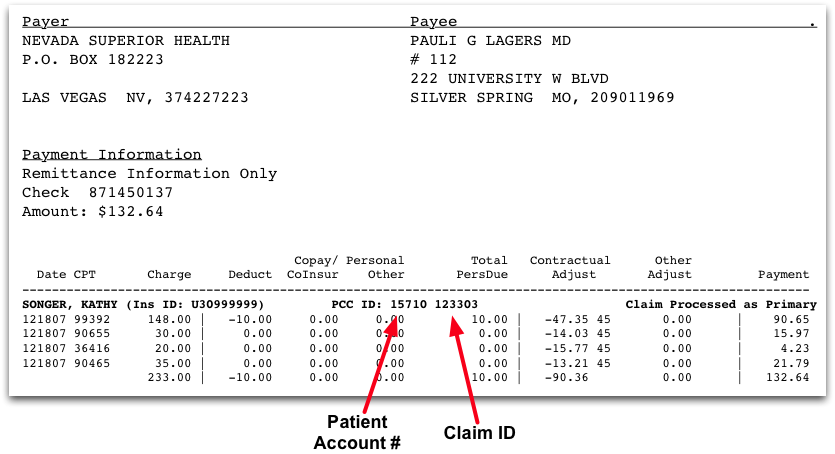
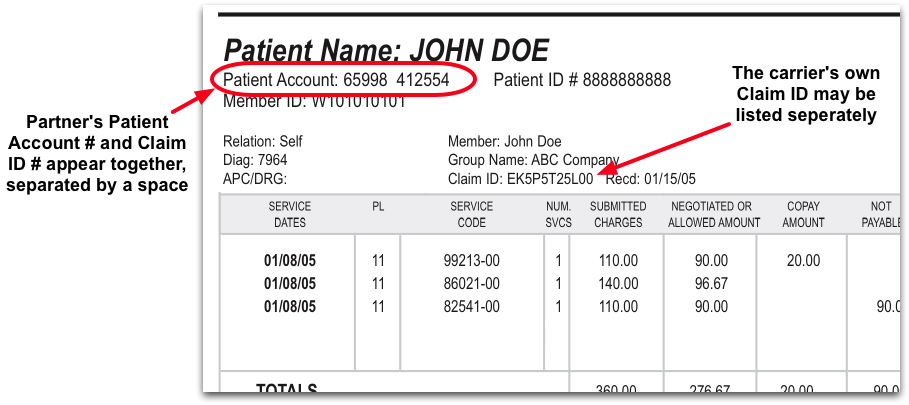
Find the Claim ID on Reports and EOBs
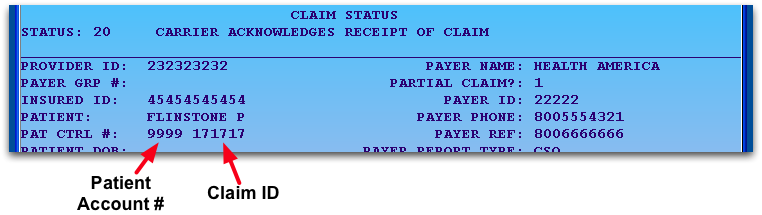
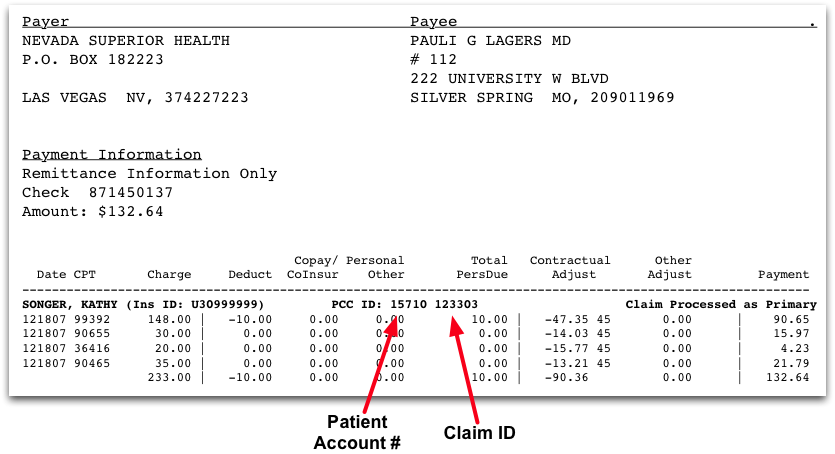
While your PCC system can identify the Claim ID quickly and easily, different reports and EOBs may display the claim ID in different ways. Below are some examples.
Posting Payments and Adjustment
For most claims, your PCC system will automatically identify the claim ID and post incoming payments and adjustments for you. However, if you need to post a payment or adjustment manually, the Post Insurance Payments (pip) program can ask you for the claim ID. If you can find it on the EOB and enter it, you will be able to post payment and adjustments faster, as the program will pre-selecting the specific charges for that claim. But don't worry! If you can not find the claim ID for some reason, you can always press Enter and search by patient name, birthdate, phone number, or other information.
Related Articles
-
CARC Values in Practice Management
When insurance carriers send payment and adjustment information, either on an EOB or an ERA, they often include a code with a small message. These codes are known as CARC values, or Claim Adjustment Reason Codes, and they are an industry-wide standard.
-
What is a Claim ID Number?
Every insurance claim in Partner has a unique identification number. The number appears in various Partner reports and programs, and you can use it to improve claim tracking and payment posting.
-
Submit Claims
Follow this procedure to prepare and send claims.
-
Insurance Billing Overview
Partner's insurance billing tools help submit claims, review rejections, and work down your insurance accounts receivable. Partner helps you maximize the use of your time as you pursue proper insurance reimbursement.
-
Check Eligibility in Partner
You can review and confirm patient insurance eligibility in either PCC EHR or in the Partner practice management system. This article teaches you how to use Partner's eligibility program to review status for upcoming appointments.
-
Print Paper HCFA Claim Forms
Hopefully most of your claims are submitted electronically. Some claims must still be printed on paper, however. The procedure above provides the basics. This section describes additional details and options in the hcfa program.
-
The Claim Journey Explained
How is a claim created, and what happens in the background to make sure your practice is paid? Read below to learn some of the "under the hood" workings of claims after you post charges into PCC EHR.
-
Check Patient Insurance Eligibility
PCC automatically checks insurance eligibility for all of a scheduled patient's active insurance plans, if the carriers support automated eligibility. You can use eligibility features in PCC to review and confirm eligibility for upcoming appointments. You can also review and re-check a patient's insurance eligibility status during Patient Check-In.
-
Accounting Challenges
The medical biller's job would be easier if accounts paid on time and insurance companies reimbursed the correct amount. Unfortunately, accounts build up balances and credits and insurance companies overpay, underpay, and demand "takebacks."
-
Configure Procedure and Diagnosis Billing in PCC EHR
Use the Billing Configuration tool to configure billing behaviors of procedures and diagnoses and the Billing screen in PCC EHR. Follow the procedures below to open the Billing Configuration tool and make changes.
-
Review Policies in Practice Management and Add an Insurance Plan to Your System
This is a placeholder for the article excerpt, a one or two sentence summary.
-
Set a Default Billing Place of Service for Telemedicine Visits
When you schedule and perform a telemedicine visit, it makes sense to use your office location—the doctors can see their whole schedule, and your practice can see what's happening at a glance. When it's time to bill, however, some carriers require a special telemedicine place of service. It can be cumbersome to manually switch the […]
-
Insurance Billing (Advanced Training Session)
Watch this video to learn insurance billing workflows for configuration, claim review, and reporting.
What Is a Claim Number for Insurance
Source: https://learn.pcc.com/help/what-is-a-claim-id-number/#:~:text=Every%20insurance%20claim%20in%20your,claim%20tracking%20and%20payment%20posting.
0 Response to "What Is a Claim Number for Insurance"
Post a Comment